Stimulated by Chen et al 2024.[1]
TEAS – transcutaneous electrical acupoint stimulation (ie a form of TENS)
TENS – transcutaneous electrical nerve stimulation
CVA – cerebrovascular accident
IF – impact factor
RCT – randomised controlled trial
ICU – intensive care unit
GCS – Glasgow coma scale
GI – gastrointestinal
NG – nasogastric
CD – cluster of differentiation
CD4 – protein marker for helper T cells, but also present on some phagocytes
CD8 – protein marker for cytotoxic T cells– key to acronyms
This paper came out in early December 2024, so I have been sitting on it for a month or so. I do not highlight TEAS very much on this blog – there are only 2 previous blogs with TEAS in the title: TEAS anyone? and TEAS vs dexamethasone in PONV.
It is published in the Journal of Investigative Surgery (IF 2.1), which has been around since the late 1980s, and became fully open access in 2023. The editorial board is global but principally from the US and Europe. There is one member from mainland China.
The paper reports quite a big RCT (n=300) with 2 parallel arms. The patients had all undergone surgery following CVA and were admitted to the ICU with the expectation of remaining there for at least a week. Surgery following CVA is relatively uncommon and usually only required in haemorrhagic strokes, which make up about 13% of all CVAs. 20-30% of patients with intracerebral haemorrhage require surgery.
The patients in this trial were described as having severe CVAs requiring surgery and subsequent care on ICU with mechanical ventilation and a GCS score of 3 to 8. In such patients, post-operative recovery of gastrointestinal motility, subsequent nutrition, and immune function can be significantly compromised. This is where the TEAS came in…
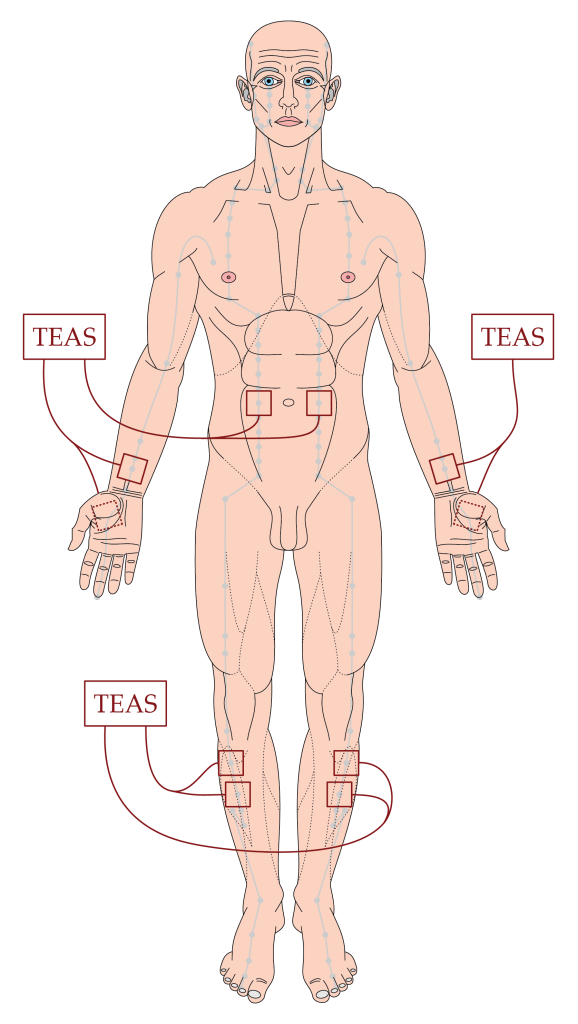
TEAS was applied via 40mm square TENS pads to pairs of points on each limb and on the abdomen – PC6 to LI4, ST36 to ST37, and ST25 to ST25 on each side. The HANS-200A device was used, which has two outputs, so 3 devices were needed for one patient. TEAS was applied twice a day for 2 weeks. Each session entailed 30 minutes stimulation at a frequency of 2/100Hz and an intensity just sufficient to cause ‘slight muscle contraction or tremor’.
The sham group had exactly the same intervention but without any electrical stimulus. They were informed that points were stimulated with a ‘microcurrent’ and that this may result in no sensation or a very mild sensation.
There does not seem to be a primary outcome nominated, but there were a lot of parameters recorded, as you might expect in any patient in ICU following brain surgery. GI motility was monitored by a variety of standard metrics such as time to first defaecation, but before that, since all patients were feed via an NG tube following a standard regime of enteral nutrition, gastric residual volume was an early metric of GI function. Nutritional status was monitored by blood values of prealbumin, albumin, haemoglobin, and total protein. Immune function was monitored via levels of various immunoglobulins and the CD4/CD8 ratio. These blood values were recorded on days 1, 3, 7, 10, 14, and at 1, 3, and 6 months post-surgery.
Recruitment took 30 months from January 2021 to June 2023, and uptake was good, with only 315 screened to achieve the desired recruitment target of 300. There was no mention of any patients being unwilling to join the trial.
60% of patients were male and the average age was 59 years. Baseline parameters were all well balanced between the groups. Nutritional markers all improved significantly faster in the TEAS group from day 3, 7, or 10 depending on the specific parameter. Similarly, blood levels of immunoglobulins (apart from IgE) and the CD4/CD8 ratio fell faster in the TEAS group than the sham TEAS group from day 7.
The median time spent in ICU was 2 days shorter for the TEAS group and the total hospital stay was 13 days shorter. Stroke rehabilitation indices were improved, adverse events were lower, and readmission rates were halved in the TEAS group.
References
1 Chen Y, A S, Liu C, et al. A Randomized Controlled Trial Assessing the Impact of Transcutaneous Electrical Acupoint Stimulation on Gastrointestinal Motility, Nutritional Status, and Immune Function in Patients Following Cerebrovascular Accident Surgery. J Invest Surg. 2024;37:2434093. doi: 10.1080/08941939.2024.2434093
You must be logged in to post a comment.