Stimulated by Liu et al 2025.[1]

TCM – traditional Chinese medicine (acupuncture and CHM)
CHM – Chinese herbal medicine
MwoA – migraine without aura
RCT – randomised controlled trial
MMD – monthly migraine days (from a 4-week headache diary)
EA – electroacupuncture
RR50 – responder rate 50 (a 50% or more reduction in MMD)
NMA – network meta-analysis– key to acronyms
This is the 387th blog post on this site and the first one to include TCM in the title. The paper I am highlighting this week is a moderately large (n=212) head-to-head (parallel arm) RCT of acupuncture plus Chinese herbal medicine versus flunarizine in the prophylaxis of episodic migraine (all were classified as MwoA).
I highlighted a sham controlled trial of acupuncture in MwoA just recently – Acupuncture for MwoA 2025. This was a similar size (n=198) and seems as though it was a similar population, although the baseline MMD was a little higher in the current trial (6.2 vs 4.7).[2]
Flunarizine is a calcium channel blocker like verapamil, but they are different types of molecular structure (diphenylpiperazine vs phenylalkylamine) and target calcium channels in different cell types to different degrees (neuronal vs cardiovascular). Flunarizine is not licenced in the UK or US because it did not pass regulatory review. This seems more to do with timing than efficacy or safety issues, but flunarizine does also block the dopamine D2 receptor, and this can eventually induce parkinsonism as well as depression and mood changes.
Flunarizine is used a lot in China, where it is considered first-line in migraine prophylaxis. So, it does seem like a very suitable comparator for the TCM treatment approach, particularly if you are keen to increase the market share for the latter.
In this trial, flunarizine was used in a dose of 10mg per day for 4 weeks. The drug was then stopped and the patients followed up at weeks 8, 12 and 16.
The TCM treatment involved 12 (30-minute) sessions of acupuncture over 4 weeks and 2 packets of herbal granules (XZDL decoction) a day for 4 weeks. The acupuncture included obligatory points (GV20, GB20, GB8) and adjunct points (TE5 and GB34, LI4 and ST44, BL60 and SI3, or LR3 and PC6 respectively) based on the typical position of the headache (temple, forehead, occiput, or vertex respectively). EA at 2/100Hz was connected across the points at GB20 and at GB8. The intensity was set between 0.1 to 1.0mA based on the perception and tolerance of the patient.
The primary outcome was the change from baseline in MMD during the 4-week treatment period. This seems a little too quick to get the best effect from acupuncture since it will be 2 weeks in to recording the outcome before you have done enough sessions to constitute a reasonable course of treatment to evaluate. However, in terms of drug or herbal effects it is more relevant to look at the peroid of consumption, and since both were stopped at 4 weeks, this outcome point does not disadvantage the drug or herbal interventions.
Note that in the last blog on MwoA (link above), the trial used change from baseline in migraine frequency rather than MMD and chose a longer duration (from baseline to trial end at 16 weeks, which means until the 12 to 16 week diary).
From baseline (-4 to 0 weeks) to the end of treatment (0 to 4 weeks) there was a drop of 3.0 days (MMD) in the TCM group and 2.3 days in the flunarizine group. The RR50 was 57.6% and 41.5% respectively. The latter improved in the TCM group over the follow-up period as you might expect, since the influence of 12 sessions of acupuncture is likely to last several months if not longer. At the 16-week point the RR50 had risen to over 70% in the acupuncture group and dropped to under 30% in the flunarizine group (data from Supplement Figure 6, which differs from what is reported in the text of the paper).
I have no experience of CHM, either clinically or in terms of reading the research base, so I asked ChatGPT 5.0 to help me compare the outcomes of CHM with acupuncture, and then with all the various pharmaceutical approaches in terms of the reduction in MMDs. I did not check all the research, so the figure below should come with a veracity warning, and I am using it merely to give an overall impression of the size of effects measured in the active intervention groups of RCTs.
I used the change from baseline MMD in the active groups and ignored the sham groups for obvious reasons (as stated on here previously, sham acupuncture is not the same as placebo topiramate – see Acupuncture versus topiramate in chronic migraine and the other blogs linked from 2021 and 2019). The absolute change from baseline is generally greater for groups with higher baseline values (for example chronic migraine versus episodic migraine), so ChatGPT 5.0 suggested comparing the percentage change from baseline.
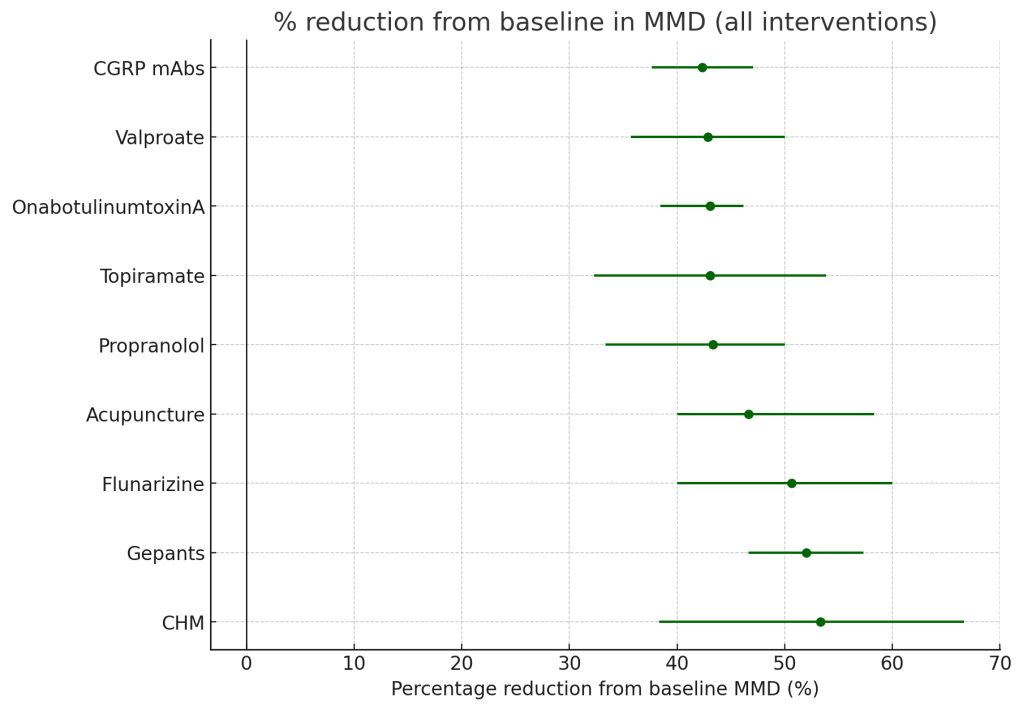
As you can see, everything seems to work to the same degree, between 40% and 55%, and this would align with the conclusion of a very large NMA published recently in Annals of Internal Medicine, which concluded that no high certainty evidence favoured one pharmacologic treatment for prevention of episodic migraine over another.[3]
The combination of acupuncture and herbal medicine used in this trial achieved a reduction of 3.7 MMD by the end of the follow-up period. That equates to a 60% reduction from baseline. For comparison, the flunarizine group achieved a ~40% reduction, which is just on the lower CI limit of what ChatGPY 5.0 came up with for the drug.
A 60% reduction in the combined group made me consider the possibility of synergy between acupuncture and CHM, but the best effects were achieved long after the herbs were stopped, and the MMD data from the previous trial,[2] where acupuncture was used alone, demonstrated a reduction of ~60% as well.
References
1 Liu L, Chen Q, Zhao L, et al. Traditional Chinese medicine versus flunarizine for the preventive treatment of episodic migraine: a randomized controlled clinical trial. QJM. 2025;hcaf210. doi: 10.1093/qjmed/hcaf210
2 Sun M, Xie C, Wang Y, et al. The Prophylactic Effect of Acupuncture for Migraine Without Aura: A Randomized, Sham-Controlled, Clinical Trial. J Evid-Based Med. 2025;e70059. doi: 10.1111/jebm.70059
3 Damen JAA, Yang B, Idema DL, et al. Comparative Effectiveness of Pharmacologic Treatments for the Prevention of Episodic Migraine Headache: A Systematic Review and Network Meta-analysis for the American College of Physicians. Ann Intern Med. 2025;178:369–80. doi: 10.7326/ANNALS-24-00315
You must be logged in to post a comment.