Stimulated by Schlaeger et al 2026.[1]
RCT – randomised controlled trial
IF – impact factor
TYN – Takakura and Yajima needle
MPQ – McGill pain questionnaire (computerised version)
PINS – pain intensity number scale (0–10)
API – average pain intensity (mean of current, least and worst in 24 hours)
MCID – minimal clinically important difference– key to acronyms
Judith Schlaeger is an academic nurse midwife based at the University of Illinois Chicago (UIC). She is the only Schlaeger publishing in the acupuncture field, and she has been on the authorship of a bunch of (8) papers in Acupuncture in Medicine (IF 2.6). I remember her name from the first RCT of acupuncture in vulvodynia, which was published in 2015.[2]
Before her 2015 paper, published in the Journal of Sexual Medicine (IF 3.3), there was little published on acupuncture in vulvodynia, and I had to rely on a well reported cohort of 12 women from the late 90’s to justify trying the treatment in clinical practice.[3] Schlaeger’s 2015 paper was a waiting list controlled RCT (n=32). The one just out is larger and sham controlled (n=89) and even attempts to be double blind (ie to blind the practitioners as well as the patients). This paper is published in The Journal of Pain (IF 4.0), the official journal of the US Association for the Study of Pain (USASP), as opposed to the journal Pain (IF 5.5), the official journal of the International Association for the Study of Pain (IASP).
Attempting to blind the acupuncturists can mean only one thing – they must have used the Takakura needle.
The Takakura and Yajima needle (TYN) was indeed a clever innovation in the late noughties,[4,5] taking forward elements of the famous Streitberger needle from the decade before,[6,7] and the Park sham device,[8,9] which followed close on Konrad’s heels (Konrad Streitberger). The major drawback from the perspective of northern Europe, where we like to needle deep into muscle tissue and often carry a reasonable layer of spare energy under our skin (in the form of subcutaneous fat), is that the active version of the TYN penetrates a maximum of 5mm. So, in most northern European acupuncture points, the tip will not actually reach to even the most superficial muscle.
So, this was a sham controlled, potentially double blind acupuncture RCT with a non-penetrating sham but a rather gentle and superficial real acupuncture treatment. Oh, as well as being only 5mm deep, the TYN is just 0.16mm in diameter.
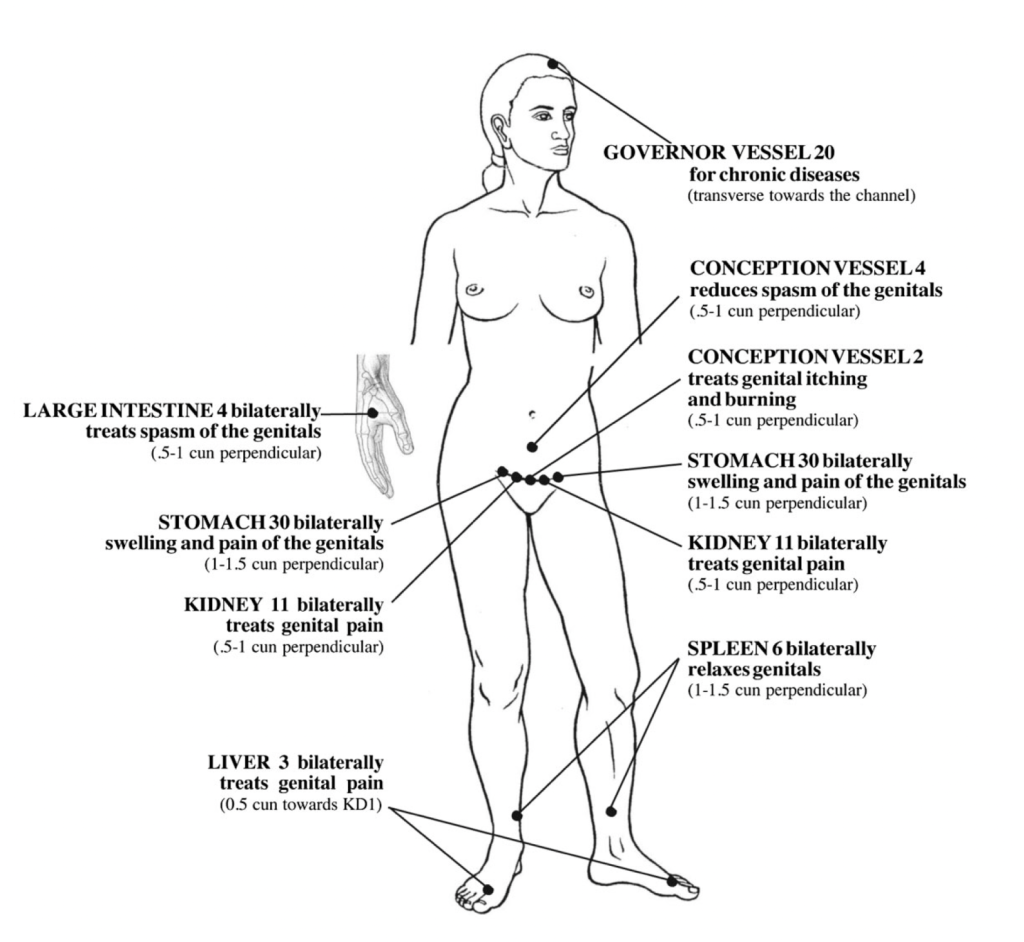
The protocol was the same as for the 2015 paper, with the same diagram of the points, which I quite like (see above). I’ll go through the points from top to bottom… GV20 might just do something with 5mm depth of a red needle. Similarly, at LI4, the needle tip should penetrate muscle by a few millimetres. Next we get to the abdomen, with CV4 and 5 points along the top of the pubis (CV2, KI11, ST30). None of these are going to reach muscle. Finally, in the lower limbs we have SP6 and LR3. The latter point might just touch something below the fat layer, but definitely not at SP6 in an adult female ankle. So, in summary, we might just have some gentle but relevant needling at one bilateral segmental point (LR3), and some general effects from 3 other points (GV20 and bilateral LI4).
Treatment sessions were twice a week for 5 weeks, which was good. The primary outcome was vulvar pain measured with MPQ and PINS. The latter is an acronym rather than an implement. Ouch at the thought! Average pain intensity (API) was calculated as the mean of current pain intensity and the least and worst pain in the previous 24 hours.
The second phase of the trial was for evaluating the length of the effect in women that responded during the treatment phase. The outcome used here was the tampon test – PINS was measured immediately after insertion of an unlubricated tampon. This was performed weekly for 12 weeks or until the PINS returned to baseline.
Given what I have said about the active treatment, it will be no surprise that the context of care probably had a much bigger impact than the actual penetrating needling. There was a clinically relevant reduction in pain in both groups but no difference between them.
The MCID used for provoked pain (PINS after tampon insertion) was taken as 1.5 and 57% of women achieved this at the end of the treatment phase. Over the subsequent 12 weeks a much higher proportion of the sham group returned to baseline pain (>50%) compared with the penetrating acupuncture group (~30%). This difference was significant.
So, we have a very small signal suggesting that shallow penetrating acupuncture with fine needles performed 10 times in 5 weeks has an effect on provoked vulvodynia that outperforms an elaborate sham.
Unfortunately, the device was not successful at consistently blinding the practitioners or the patients in the penetrating acupuncture group of this trial, although blinding was maintained in the placebo group. Expectations of subjects were not evaluated, so it leaves us wondering whether the marginally better effects in the penetrating acupuncture group could be attributed to enhanced expectation derived from unblinding of both patients and practitioners in this group.
References
1 Schlaeger JM, Steffen AD, Takakura N, et al. Long-lasting effect of penetrating acupuncture among responders: Double-blind RCT of acupuncture for vulvodynia. J Pain. 2026;38:105584. doi: 10.1016/j.jpain.2025.105584
2 Schlaeger JM, Xu N, Mejta CL, et al. Acupuncture for the treatment of vulvodynia: a randomized wait-list controlled pilot study. J Sex Med. 2015;12:1019–27. doi: 10.1111/jsm.12830
3 Powell J, Wojnarowska F. Acupuncture for vulvodynia. J R Soc Med. 1999;92:579–81. doi: 10.1177/014107689909201110
4 Takakura N, Yajima H. A double-blind placebo needle for acupuncture research. BMC Complement Altern Med. 2007;7:31. doi: 10.1186/1472-6882-7-31
5 Takakura N, Yajima H. A placebo acupuncture needle with potential for double blinding – a validation study. Acupunct Med. 2008;26:224–30. doi: 10.1136/aim.26.4.224
6 Streitberger K, Kleinhenz J. Introducing a placebo needle into acupuncture research. The Lancet. 1998;352:364–5. doi: 10.1016/S0140-6736(97)10471-8
7 Kleinhenz J, Streitberger K, Windeler J, et al. Randomised clinical trial comparing the effects of acupuncture and a newly designed placebo needle in rotator cuff tendinitis. Pain. 1999;83:235–41. doi: 10.1016/S0304-3959(99)00107-4
8 Park J, White A, Lee H, et al. Development of a New Sham Needle. Acupunct Med. 1999;17:110–2. doi: 10.1136/aim.17.2.110
9 Park J, White A, Stevinson C, et al. Validating a new non-penetrating sham acupuncture device: two randomised controlled trials. Acupunct Med. 2002;20:168–74. doi: 10.1136/aim.20.4.168
You must be logged in to post a comment.