Stimulated by Pinheiro et al and Yi et al 2026.[1,2]
MSK – musculoskeletal
IF – impact factor
MRI – magnetic resonance imaging– key to acronyms
This week I have chosen a couple of recent anatomical papers that examine innervation patterns in the two lower limb muscles named in the title of this blog. The studies are a little different in methods, but the intention is the same – to find the most likely location of trigger points that can be treated by needling or injection.
Gluteus medius is the more common site for trigger points and other MSK pathology (tendinopathy or tears). It is one of the two muscles that I use to test the muscular integrity of anatomical resources. Gluteus medius must have the record for the most inaccurate representations of all human muscles. Less than ~1% of images online are accurate representations of the contractile elements of this muscle (excluding images from dissection of course), and the ones that are accurate are usually copies of the graphic drawn by Barbara D Cummings in The Trigger Point Manual.[3,4] This is a beautiful and highly accurate representation, and the authors include a poorer reproduction of this image. Ironically, as if to prove my point, they then include a further representation of the muscle that is entirely inaccurate directly below. This does not affect the data in their paper, but it is like an eyesore to me.
The authors, who are from São Paulo, and published their report in Biomedical Research International (IF 2.3), performed dissections of 20 gluteus medius muscles from 10 human cadavers and carefully identified all the nerves supplying the muscle. They counted the number of nerves in each quadrant of the muscle and reported this, which is useful. Their idea was to examine the correlation with the position of the X’s in the original trigger point manual.[3] This is a rather flawed idea, since the X’s were just examples of possible common positions, they were never meant to be taken as the only positions for trigger points. I remember Bob Gerwin telling me years ago that they were considering removing the X’s altogether because of this sort of misinterpretation, and sure enough the 3rd edition of The Trigger point Manual has no X’s.[4] Bob’s forward in that edition explains that the whole muscle must be examined for trigger points.
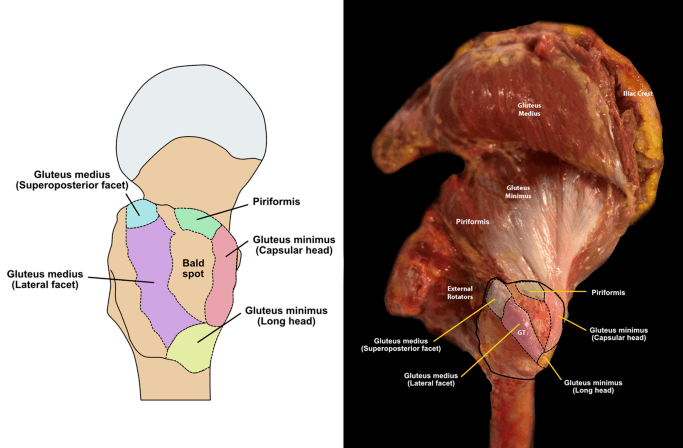
The majority of nerve entry points were in the upper posterior and lower anterior quadrants – exactly where you might expect them from the appearance of the contractile elements of an accurately represented muscle, such as that produced by Barbara.
The useful cadaveric image above was found for me by ChatGPT5.2, but it was not able to tell me exactly where the image came from. When I asked for a citable reference, I was given a well cited paper from the journal Radiology (IF 15.2),[5] but the images in this paper all appear to be of MRI scans, and the title suggests it was more focussed on bursae than gluteus medius attachments, although the two are clearly related.
Moving on to the paper on soleus, published in Scientific Reports (IF 3.9), this group used a technique we have discussed here before – Sihler’s staining (see Where to needle 2022 and Where to needle 2023 and Where to needle – part 3). It is the same group as all the previous papers using the technique that I have highlighted. They seem to be getting quicker at performing the Sihler’s staining. In the first paper I highlighted from 2022, the method took about 3 months, then this reduced to 5 weeks in the paper from 2023. In the current paper, they have got it down to about 3 weeks.
The group are interested in finding the most extensive arborisation patterns of nerves within the muscle so that they know the best targets for botulinum toxin injection, but these sites are also likely to be the best areas for finding trigger points, since the endplate zones will be close by.
I was gratified to see that the crosshatches on the BMAS trigger point chart for the soleus muscle match well to the zones described in this paper. No doubt I positioned them by looking at The Trigger Point Manual, which brings us back to whether or not we should have X’s (or the superior crosshatch symbol) at all. No doubt we will discuss this further at the webinar tonight.
References
1 Pinheiro RP, Macaya DAM, Itezerote AM, et al. Anatomical Investigation of the Gluteus Medius Muscle Innervation and Its Topographical Correspondence With Myofascial Trigger Points. BioMed Res Int. 2026;2026:7544057. doi: 10.1155/bmri/7544057
2 Yi K-H, Hu H, Hwang S-O, et al. Intramuscular neural distribution of the soleus for botulinum neurotoxin injection: application to spasticity. Sci Rep. 2026;16:279. doi: 10.1038/s41598-025-07508-2
3 Travell JG, Simons DG. Myofascial Pain & Dysfunction. The Trigger Point Manual. Volume 2. The Lower Extremities. 1st ed. Baltimore: Williams & Wilkins 1992.
4 Donnelly JM, Fernandez de las Peñas C, Finnegan M, et al., editors. Travell, Simons & Simons’ myofascial pain and dysfunction: the trigger point manual. 3rd ed. Philadelphia: Wolters Kluwer Health 2019.
5 Pfirrmann CW, Chung CB, Theumann NH, et al. Greater trochanter of the hip: attachment of the abductor mechanism and a complex of three bursae–MR imaging and MR bursography in cadavers and MR imaging in asymptomatic volunteers. Radiology. 2001;221:469–77. doi: 10.1148/radiol.2211001634
You must be logged in to post a comment.