Stimulated by Li et al 2025.[1]
PSD – post-stroke dysphagia
IF – impact factor
WST – water swallowing test (30mls of warm water)– key to acronyms
This is the third paper on PSD I have highlighted this year. It is a cohort study from China, which is essentially an outcomes audit with some fancy regression analyses to probe potential variables of interest in terms of improved outcomes in PSD. The paper is published in the open access journal Frontiers in Neurology (IF 2.8).
The bottom line message, although not by any means definitive, is concordant with previous mechanistic research (see EA for PSD from 2023).[2]
It was a multicentre project involving 27 hospitals in China. They enrolled 382 patients with PSD over a 30-month period. Patients were aged over 35 years with a WST of above 2 and onset of PSD within 90 days of cerebral infarction.
WST (as used in this paper):
- Grade 1 – smooth single attempt to swallow without coughing
- Grade 2 – requires 2 or more attempts to swallow without coughing
- Grade 3 – able to swallow in one attempt but with coughing
- Grade 4 – requires 2 or more attempts to swallow with coughing
- Grade 5 – frequent coughing, unable to swallow all the water
The main outcome was the recovery of swallowing function on discharge, at 90 days and at 180 days. Recovery was defined by WST grade of 2 or less.
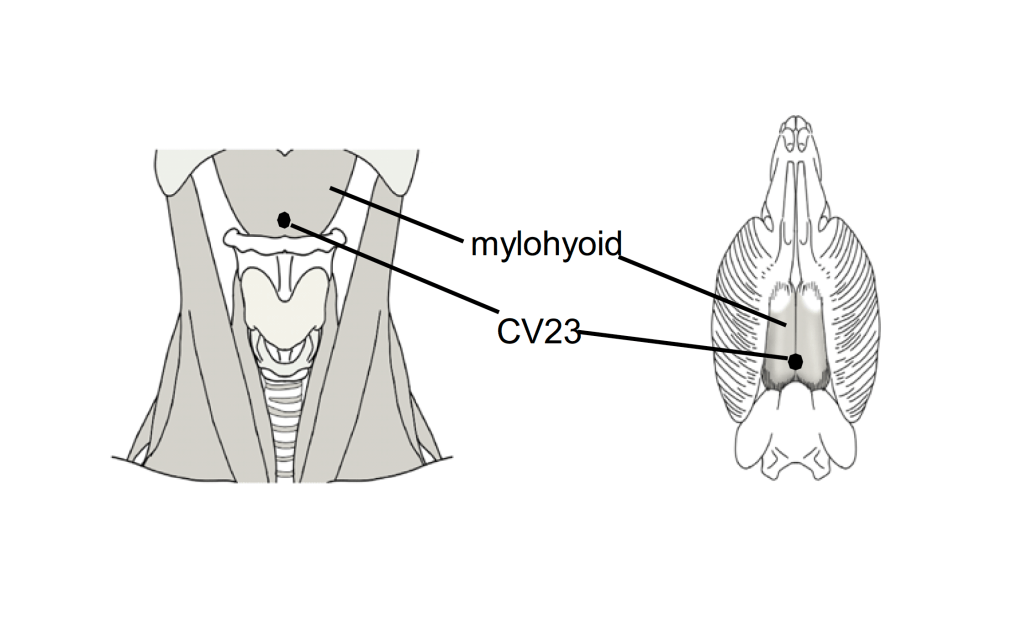
The main points used were CV23 and GB20. That all sounds fine until I tell you that GB20 was inserted 50mm to 90mm in the direction of the laryngeal prominence with the aim of stimulating a feeling of numbness or soreness in the region of the pharynx. It is theoretically possibly to reach the middle and lower pharyngeal constrictor muscles with this angulation from GB20, although that would mean passing just lateral to the zygapophyseal joint between C1 and C2 where you find the vertebral artery running up between the transverse foramina of the same vertebrae. Just anterior to this is the internal carotid artery, so if you miss the vertebral artery, you have a chance of hitting the only other artery to the brain on that side of the body.
This seems to be a colossally reckless intervention, particularly as it may not add much to the use of CV23, which we already know can prevent dysphagia entirely (see EA for PSD) in a rodent model with a very targeted stroke affecting motor control of the mylohyoid muscle.
Moving on… the results were consistent with improved effects for earlier acupuncture treatment, although multivariable analysis only showed a statistically significant adverse effect when acupuncture was not initiated in the first 4 weeks after stroke.
It was interesting to see that hyperlipidaemia and obesity were both associated with improved outcomes although there were relatively small numbers in these subgroups (68 and 35 respectively out of a total of 359 with full outcome data). Since I can rarely resist mechanistic speculation, I wonder whether an unimpeded intake of fats results in more healthy and resilient membranes in neurons of the CNS, whilst perhaps not being so good for arterial walls.
So, in summary, this paper is not as convincing as I first thought when I selected it; however, it does provide some indication that early acupuncture is beneficial in the recovery of swallowing function after stroke, which is intuitively sensible and consistent with both mechanistic data (see EA for PSD) and other clinical outcomes in the world of acute neurological conditions (see SAH headache 2019).
References
1 Li J, Li G, Wang S, et al. Early acupuncture intervention strongly associates with improved swallowing recovery in post-stroke dysphagia: a multicenter real-world cohort study. Front Neurol. 2025;16:1553947. doi: 10.3389/fneur.2025.1553947
2 Yao L, Ye Q, Liu Y, et al. Electroacupuncture improves swallowing function in a post-stroke dysphagia mouse model by activating the motor cortex inputs to the nucleus tractus solitarii through the parabrachial nuclei. Nat Commun. 2023;14:810. doi: 10.1038/s41467-023-36448-6
You must be logged in to post a comment.