Inspired by Xian et al 2022.[1]
SR – systematic review
key to acronyms
EA – electroacupuncture
RCT – randomised controlled trial
APACHE – acute physiology and chronic health evaluation
APACHE II – a score applied to patients on admission to ICU for risk stratification
ICU – intensive care unit
MD – mean difference
CI – confidence interval
I saw this paper as a proof a couple of weeks ago and have been waiting to highlight it here ever since.
This is the first paper to demonstrate a reduction in mortality from acupuncture in humans
It is the first paper to demonstrate a reduction in mortality from adjuvant acupuncture in humans with sepsis. Ever since the first mortality outcome was reported in 2014 in laboratory research,[2] I have been wondering when we would see this. There is a plausible mechanism and a dramatic effect in the animal models, so it was just a matter of time before we saw evidence of reduced mortality in humans.
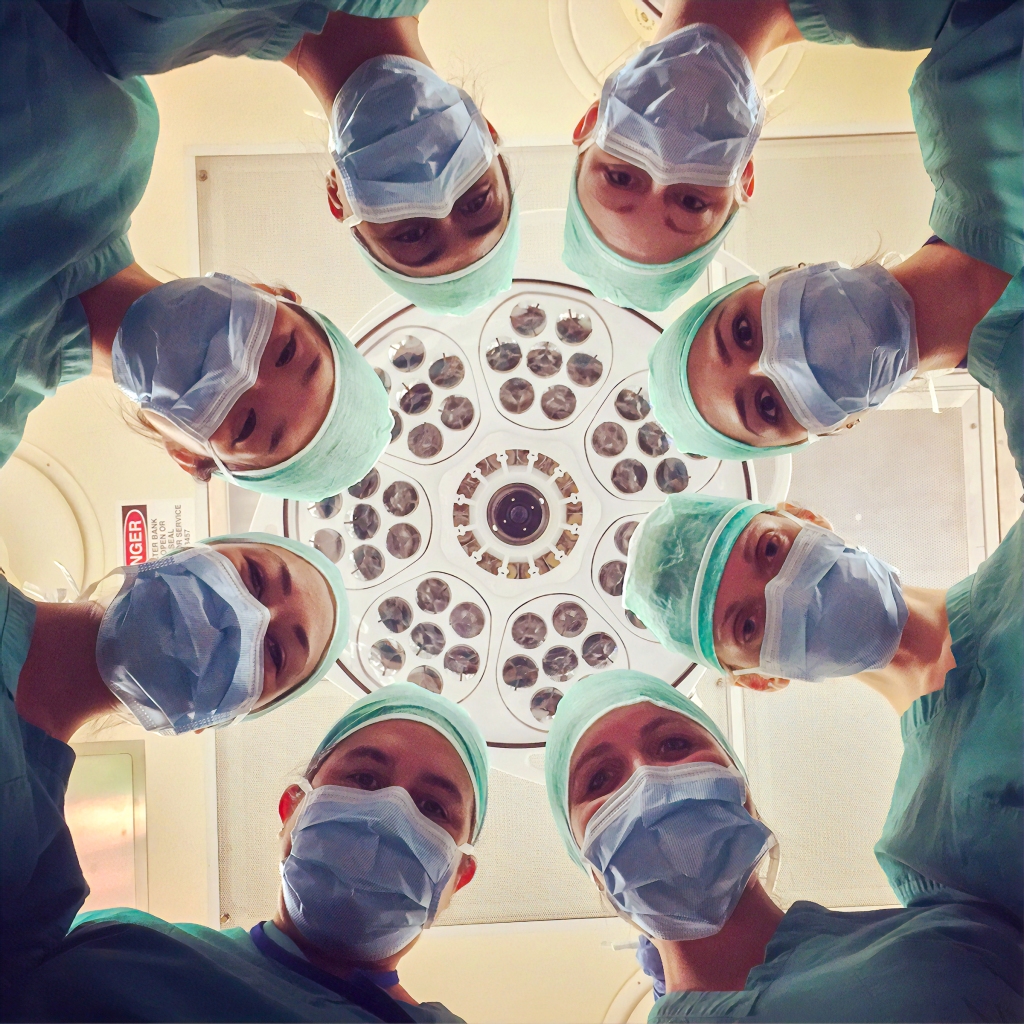
This is an SR from Shandong University, and unsurprisingly all the included RCTs come from China. I did offer to try some ST36 EA in ICU at the start of COVID in the UK, but equally unsurprisingly that offer was not taken up.
I don’t remember seeing a paper from Shandong University in our journal before, so I looked up the place. It is one of the largest universities in China with 57.5k students in 2009. Shandong is a coastal province south of Beijing and north of Nanjing (and Shanghai). It has a large peninsular jutting into the Yellow Sea directly towards North Korea. The university is distributed across the large centres in the region, so the Jinan campus, from where this paper derives, is over 500km from the most eastern campus in the coastal city of Weihai, formerly Weihaiwei.
The SR included 17 RCTs with 1099 patients. There were 22 reports of these 17 RCTs and only 3 reports were in English. The rest were in Chinese. The two primary outcomes were mortality and the APACHE II score.
The APACHE II score was developed in the 1980’s,[3] and despite further versions being developed (eg III & IV),[4] version II is still the most widely used, probably because it is the easiest and it fits on one side of a single page. A recent paper suggests that the APACHE II score on day 3 is the best predictor of outcome in ICU patients, with a score of 17 being the best cut-off for defining patients at high risk of mortality.[5] Technically the score can go up to 74, but most patients do not get far above 34 and remain alive.
Nine RCTs including 490 patients provided mortality data at day 28. Meta-analysis of this data favoured routine care plus acupuncture compared with routine care alone with an odds ratio of 0.69. That is more than a 30% reduction in mortality associated with the addition of acupuncture.
There was more than a 30% reduction in mortality associated with acupuncture
Eleven RCTs including 720 patients provided APACHE II data at day 7. Additional acupuncture was associated with a lower score (MD: -2.84; 95% CI: -4.09 to -1.58). The significant heterogeneity in this result was entirely explained by a single outlying RCT, removal of which in sensitivity analysis resulted in an increase in the difference in APACHE II score to more than 3 points.
Of 13 secondary outcome measures of disease severity, 7 showed very highly significant differences and 2 more showed significant differences between groups at day 7. As would be expected, most of the markers for inflammation were reduced with acupuncture. T lymphocyte counts changed with a significant increase in the percentage of CD3+ and CD4+ but not CD8+ cells. This seems to represent an increase of T helper cells more than T cytotoxic cells, and the former probably include the splenic T helper cells that are required for part of the vagal anti-inflammatory mechanism discussed in last week’s blog.
GRADE levels for all outcomes were low or very low due principally to risk of bias from a lack of blinding and the overall sample size in meta-analysis. Having said that, most of the outcomes are objective and unlikely to be influenced by expectation. It has been suggested that blinding is not important where outcomes are objective – see previous blog: Blinding – where is the bias? In terms of the total sample size, I would have to agree that to be certain about a mortality outcome we would ideally want tens of thousands rather than just under 500. Hopefully this first SR demonstrating reduced mortality will stimulate some interest and open some ICU doors to considering research on acupuncture. The key risk to adoption of this cheap intervention in the west is the development and marketing of hugely expensive patented alternatives that do the same thing but are backed by the lobbying power of the commercial sector. For an example of this development, see the previous blog: Implanted pigs.
ST36 was used in 15 of the 17 RCTs
I nearly signed off without mentioning ST36 EA! Well, ST36 was used in 15 of the 17 RCTs and EA was used in 7 of them. Sessions of acupuncture were performed once a day in 6 RCTs and twice a day in 10. In the remaining trial 14 sessions were applied over 3 days. This was the outlier in terms of APACHE scores. There were no big differences between 1 and 2 sessions per day for the main outcomes, but some of the secondary outcomes seemed to favour 2 sessions per day, which may not be a surprise considering these outcomes were all measured on day 7, and we already know that the total number of sessions frequently makes a difference in acupuncture research.
References
1 Xian J, Wang L, Zhang C, et al. Efficacy and safety of acupuncture as a complementary therapy for sepsis: a systematic review and meta-analysis. Acupunct Med 2022;:9645284221086288. doi:10.1177/09645284221086288
2 Torres-Rosas R, Yehia G, Peña G, et al. Dopamine mediates vagal modulation of the immune system by electroacupuncture. Nat Med 2014;20:291–5. doi:10.1038/nm.3479
3 Knaus WA, Draper EA, Wagner DP, et al. APACHE II: a severity of disease classification system. Crit Care Med 1985;13:818–29.
4 Zimmerman JE, Kramer AA, McNair DS, et al. Acute Physiology and Chronic Health Evaluation (APACHE) IV: hospital mortality assessment for today’s critically ill patients. Crit Care Med 2006;34:1297–310. doi:10.1097/01.CCM.0000215112.84523.F0
5 Tian Y, Yao Y, Zhou J, et al. Dynamic APACHE II Score to Predict the Outcome of Intensive Care Unit Patients. Front Med 2021;8:744907. doi:10.3389/fmed.2021.744907
You must be logged in to post a comment.