Inspired by Huang et al 2023.[1]
EA – electroacupuncture
key to acronyms
TKA – total knee arthroplasty
RCT – randomised controlled trial
VAS – visual analogue score
PCA – patient-controlled analgesia
MSK – musculoskeletal
SD – standard deviation
CI – confidence interval
MCID – minimum important clinical difference
This is a paper that we (Acupuncture in Medicine) published online at the very end of 2023, so when it is selected for an issue, it will be 2024. If you are a BMAS member you need to access the full text via the Acupuncture in Medicine page of the BMAS website.
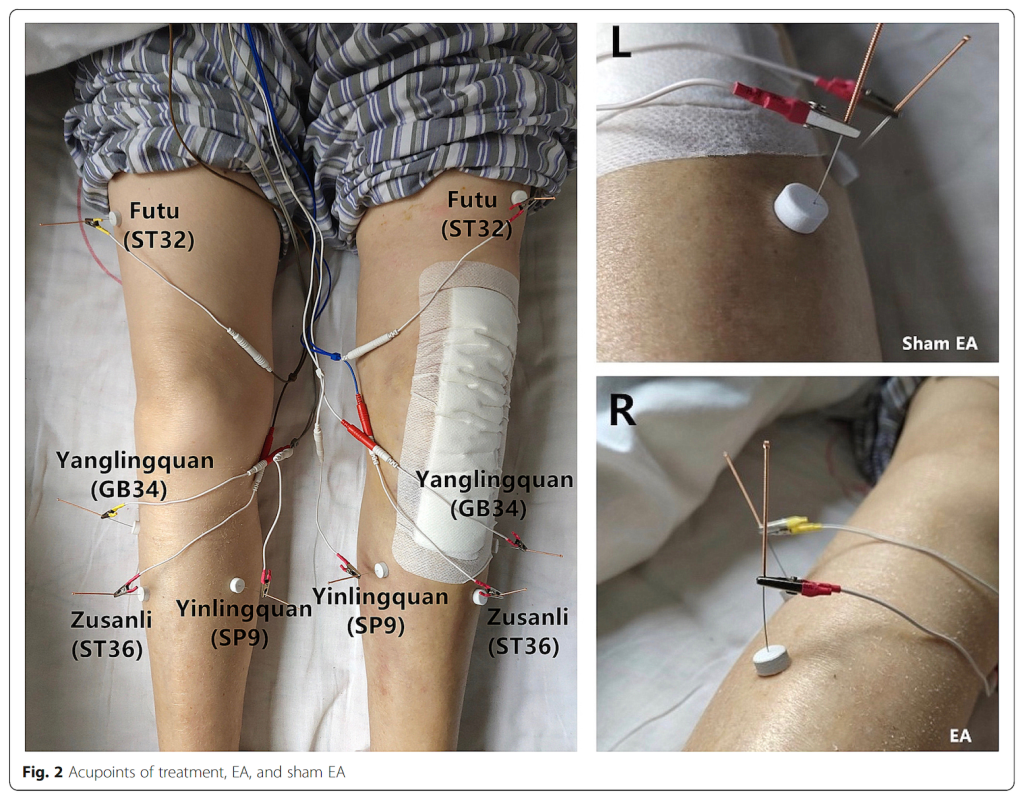
It is a 3 arm RCT with a non-penetrating sham control in one of the 3 arms. The sham involved use of a relatively small white foam disc (10mm diameter, 5mm height) placed over the points. A short blunt needle (0.30mm x 15mm) was used in the sham group and a standard needle (0.30mm x 40mm) was used to pierce through the disc and into the points in the real EA groups. This has become popular in China in recent years and seems to be quite successful. The 2 active arms compared ipsilateral with contralateral EA around the knee joint. It is not a huge trial, but I think the results would change my practice… and I don’t say that very often!
The research comes from Shanghai, and the protocol was published in 2020 along with some very useful pictures of the EA protocol as well as the sham equipment.[2]
The EA protocol connected ST32 to ST36 and SP9 to GB34 according to the image in the Trials publication, although the text in both papers mention a slightly different arrangement, presumably in error. A low frequency (2Hz) was applied at a relatively low intensity of 1mA and a pulse width of 250μs for 30 minutes on days 1, 2, and 3 post-op. Outcomes were measured at baseline, after EA on days 1, 2, and 3, and at follow-up on day 5, 7, and 10.
The primary outcomes were VAS pain during walking or joint movement at all time points and additional PCA doses recorded on day 2.
So, this is a straightforward EA protocol applied daily post-op for just 3 days. It seems quite achievable even in the West, dare I say.
114 patients with an average age of 68 were randomised to 3 groups in a 1:1:1 ratio. The power calculation was based on unpublished pilot data and aimed to determine significant superiority of the active arms over sham rather than non-inferiority of one active approach over the other, which probably would have required a larger sample size. There was no mention of testing for equivalence between the active arms, which would generally require an even larger sample size than for a non-inferiority trial.
I am not really a fan of sham controlled clinical trials, but one of the exceptions I am prepared to recommend is when EA is compared with non-penetrating EA for peripherally driven MSK pain, as in this case. The authors were also fortunate that the SDs measured on day 10 were 20% narrower than the SD they chose for their power calculation, thus they were gifted (by chance) more statistical power. Generally this works the other way around from pilot to main trial, and statistical power is lost.[3]
The sham looks convincing, and it seems as though over 70% of patients in each group thought they were getting the real treatment. It is not clear exactly how the figures for blinding were generated, although the questions detailed in the protocol seem comprehensive.
The results are pretty consistent in that both active groups were significantly better than the sham group from post-op day 2 onwards and there was no difference between the 2 active groups apart from knee circumference on day 3. The latter difference disappeared entirely during the follow-up and there was no difference in knee function between the active groups at any time point.

I confess to being a little surprised that ipsilateral EA was no better than contralateral EA despite realising many years ago that most of the effect of my EA in patients with OA knee was through effects in the spinal cord rather than local to tissues around the knee joint itself.
Given the concern about infection in joint prostheses and the fact that even acupuncture needles can, albeit rarely, cause infection through inoculation, it seems plain from this research that the contralateral approach should be recommended, at least in the immediate post-op period.
This brings me back to the business of statistical equivalence. The fact that neither active group was shown to be superior to the other is not the same as demonstrating equivalence. For equivalence we need the CIs of the difference between groups to be within one MCID of the mean for the outcome concerned.
If we take 5mm on a 0 to 100mm VAS to be the MCID, in the follow-up period on days 7 and 10, equivalence is achieved. Hence, I think I am justified to say that this trial would change my practice, if I worked in post-op rehabilitation for patients following TKA.
References
1 Huang H, Tang K, Song X, et al. Effects of contralateral versus ipsilateral electroacupuncture for analgesia and rehabilitation after unilateral total knee arthroplasty: a randomized controlled trial. Acupunct Med. 2023;9645284231211601.
2 Huang H, Song X, Zhao L, et al. Opposing needling for analgesia and rehabilitation after unilateral total knee arthroplasty: a randomized, sham-controlled trial protocol. Trials. 2020;21:385.
3 Vickers AJ. Underpowering in randomized trials reporting a sample size calculation. J Clin Epidemiol. 2003;56:717–20.
You must be logged in to post a comment.